Balancing Patient Safety and Access to Care or Anticompetitive Rhetoric?
The recent introduction of teledentistry laws in various states has sparked a heated debate within the dental community, with the American Association of Orthodontists (AAO) finding itself at the center of the discussion. As we delve into the implications of these laws and the AAO’s involvement, it becomes essential to weigh the potential benefits of technological advancements against the responsibility of safeguarding patient well-being.
Nevada is the first state to require in-person exam prior to orthodontic treatment.
This law requires “…an in-person visit before the patient begins using the orthodontic appliance” (Source AAOinfo.org website, accessed August 3, 2023). There’s something about this new law that doesn’t seem quite right. It feels like the old Andy Griffith Show, which portrays an unrealistic amount of affection and nostalgia for American small-town life. Serious real-life events like the Cuban missile crisis, President Kennedy’s assassination, the war in Vietnam and marches by African Americans for the right to vote never took place inside Mayberry’s make-believe town limits, even though all of these things were going on at the same time the show was on the air.
Serious real-life challenges like access to care and insurance reform exist in the U.S., but orthodontists seem determined to protect their own interests. I’ve been confused by and conflicted about this new law and trying to gather my thoughts and notes for the last month. I’m open to changing my mind, but my gut tells me the orthodontic profession is on the wrong side of the challenge and that history might judge us harshly.
Because many orthodontists tell me privately that they feel the same way but are afraid to speak out publicly, here are a few ideas and questions worth considering if you have the same “not-quite-right” feeling in your stomach when you read about new laws the AAO is helping draft and promote, which make it more difficult for patients to receive care in a day and age when we should be embracing teledentistry, not using it as a springboard to protect our own interests.
Balancing Risks and Benefits: Ionizing radiation, used in dental radiographs, undoubtedly poses a small but real risk to patients. Therefore, it is vital to assess whether managing a patient’s condition necessitates radiographs. The British Orthodontic Society (2015) notes that adult patients with a healthy dentition and supporting structures may undergo orthodontic treatment without radiographs. In cases where radiographs are necessary, orthodontists could order and review them asynchronously via diagnostic imaging centers and teledentistry applications.
Ethical Considerations: Healthcare practices should always adhere to ethical guidelines. The Royal College of Radiologists emphasizes that taking radiographs should never be driven by medico-legal, administrative, or precautionary reasons when there is no clinical need. It is crucial to prioritize patient well-being and avoid unnecessary procedures or tests that may not benefit the individual. How can we justify the requirement to see an orthodontist in-person and expose the patient to ionizing radiation if respected colleagues in other countries disagree?
Learning from Telemedicine: Drawing a parallel to telemedicine, I often share my personal experience with a tele-health platform for a heart condition. Through the platform, a board-certified ER physician ordered diagnostic tests and provided a comprehensive follow-up consultation. I received a superior experience and timely care, underscoring the potential benefits of telehealth technologies. If telemedicine can be effective and safe for the complex cardiovascular system, can’t it also be safe and effective for orthodontic treatment?
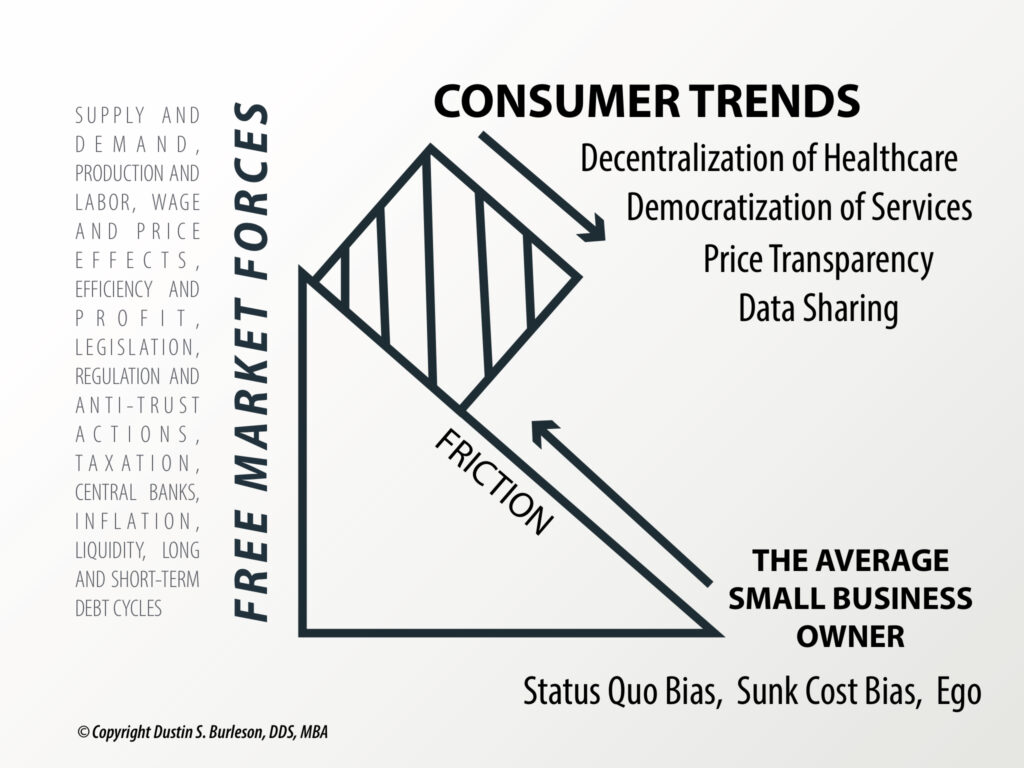
Striking a Balance: Critics argue that the AAO’s involvement in advocating for teledentistry laws might be less about patient safety and more about protecting the profession’s interests. While patient safety remains paramount, we must also consider the potential impact on access to care and competition within the dental industry. Striking a balance between patient welfare, access to quality care, and the economic interests of practitioners is a complex challenge. Orthodontists and orthodontic associations are not going to lobby state legislatures to find new ways to lower their incomes, but they need to understand how this stands in resistance of patient autonomy and the democratization of healthcare, where the trend in any free market always moves steadily towards increased access and lower costs.
Moving Forward: The orthodontic profession should establish evidence-based clinical guidelines for teledentistry through randomized, controlled clinical trials, not through the opinion of a trade association. We should compare outcomes of orthodontic patients treated with fewer or no radiographs via teledentistry versus those treated within the new protocol in Nevada’s teledentistry law. It could shed light on effectiveness and safety and we all should want to embrace this level of evidence and progress if we take ourselves seriously as doctors who want what is in the patient’s best interest. Bottom line: we can only help patients if they have access to the care we provide.
Concluding Thoughts: As the debate surrounding teledentistry laws continues, it is essential for all stakeholders to engage in constructive discussions. The future of dental care lies at the intersection of technological advancements, patient-centered practices, and professional responsibilities. Instead of fearing change, let us embrace the opportunity to adapt and evolve, ensuring that we deliver the best possible care to patients while promoting a fair and competitive healthcare landscape.
Disclaimer: The views expressed in this blog post are solely those of the writer and do not represent the position of the AAO. The intent is to encourage open dialogue and critical thinking on the topic of teledentistry and its potential impact on patient care and dental practice.

Leave a Reply